Let’s not call it cancer
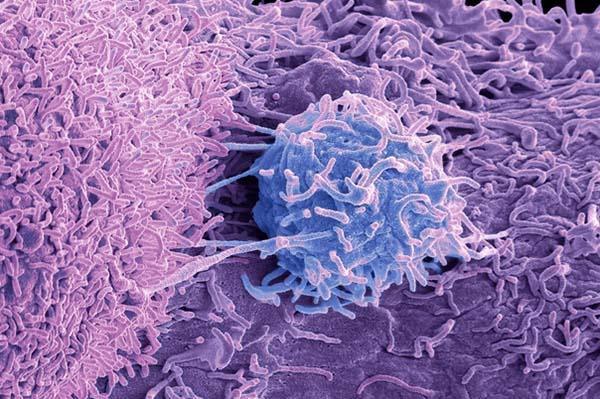
Roughly one in six men will be diagnosed with prostate cancer at some point in their lives, but these cancers usually aren’t life-threatening. Most newly diagnosed men have Grade Group 1 (GG1) prostate cancer, which can linger for years without causing significant harms.
Prostate cancer is categorized according to how far it has spread and how aggressive it looks under the microscope. Pure GG1 prostate cancer is the least risky form of the disease. It occurs frequently with age, will not metastasize to other parts of the body, and it doesn’t require any immediate treatment.
So, should we even call it cancer? Many experts say no.
Dr. Matthew Cooperberg, who chairs the department of urology at the University of California, San Francisco, says men wouldn’t suffer as much anxiety — and would be less inclined to pursue unneeded therapies — if their doctors stopped referring to low-grade changes in the prostate as cancer. He recently co-chaired a symposium where experts from around the world gathered to discuss the pros and cons of giving GG1 cancer another name.
Treatment discrepancies
GG1 cancer is typically revealed by PSA screening. The goal with screening is to find more aggressive prostate cancer while it’s still curable, yet these efforts often detect GG1 cancer incidentally. Attendees at the symposium agreed that GG1 disease should be managed with active surveillance. With this standard practice, doctors monitor the disease with periodic PSA checks, biopsies, and imaging, and treat the disease only if it shows signs of progression.
But even as medical groups work to promote active surveillance, 40% of men with low-risk prostate cancer in the United States are treated immediately. According to Dr. Cooperberg, that’s in part because the word “cancer” has such a strong emotional impact. “It resonates with people as something that spreads and kills,” he says. “No matter how much we try to get the message out there that GG1 cancer is not an immediate concern, there’s a lot of anxiety associated with a ‘C-word’ diagnosis.”
A consequence is widespread overtreatment, with tens of thousands of men needlessly suffering side effects from surgery or radiation every year. A cancer diagnosis has other harmful consequences: studies reveal negative effects on relationships and employment as well as “someone’s ability to get life insurance,” Dr. Cooperberg says. “It can affect health insurance rates.”
Debate about renaming
Experts at the symposium proposed that GG1 cancer could be referred to instead as acinar neoplasm, which is an abnormal but nonlethal growth in tissue. Skeptics expressed a concern that patients might not stick with active surveillance if they aren’t told they have cancer. But should men be scared into complying with appropriate monitoring? Dr. Cooperberg argues that patients with pure GG1 “should not be burdened with a cancer diagnosis that has zero capacity to harm them.”
Dr. Cooperberg does caution that since biopsies can potentially miss higher-grade cancer elsewhere in the prostate, monitoring the condition with active surveillance is crucial. Moreover, men with a strong family history of cancer, or genetic mutations such as BRCA1 and BRCA2 that put them at a higher risk of aggressive disease, should be followed more closely, he says.
Dr. Marc Garnick, the Gorman Brothers Professor of Medicine at Harvard Medical School and Beth Israel Deaconess Medical Center, and editor in chief of the Harvard Medical School Guide to Prostate Diseases, agrees. Dr. Garnick emphasized that a name change for GG1 cancer needs to consider a wide spectrum of additional testing. “This decision can’t simply be based on pathology,” he says. “Biopsies only sample a miniscule portion of the prostate gland. Genetic and genomic tests can help us identify some low-risk cancers that might behave in a more aggressive fashion down the road.”
Meanwhile, support for a name change is gaining momentum. “Younger pathologists and urologists are especially likely to think this is a good idea,” Dr. Cooperberg says. “I think the name change is just a matter of time — in my view, we’ll get there eventually.”
About the Author

Charlie Schmidt, Editor, Harvard Medical School Annual Report on Prostate Diseases
Charlie Schmidt is an award-winning freelance science writer based in Portland, Maine. In addition to writing for Harvard Health Publishing, Charlie has written for Science magazine, the Journal of the National Cancer Institute, Environmental Health Perspectives, … See Full Bio View all posts by Charlie Schmidt
About the Reviewer
Marc B. Garnick, MD, Editor in Chief, Harvard Medical School Annual Report on Prostate Diseases; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Marc B. Garnick is an internationally renowned expert in medical oncology and urologic cancer. A clinical professor of medicine at Harvard Medical School, he also maintains an active clinical practice at Beth Israel Deaconess Medical … See Full Bio View all posts by Marc B. Garnick, MD

Life can be challenging: Build your own resilience plan

Nantucket, a beautiful, 14-mile-long island off the coast of Massachusetts, has a 40-point resiliency plan to help withstand the buffeting seas surrounding it as climate change takes a toll. Perhaps we can all benefit from creating individual resilience plans to help handle the big and small issues that erode our sense of well-being. But what is resilience and how do you cultivate it?
What is resilience?
Resilience is a psychological response that helps you adapt to life’s difficulties and seek a path forward through challenges.
“It’s a flexible mindset that helps you adapt, think critically, and stay focused on your values and what matters most,” says Luana Marques, an associate professor of psychiatry at Harvard Medical School.
While everyone has the ability to be resilient, your capacity for resilience can take a beating over time from chronic stress, perhaps from financial instability or staying in a job you dislike. The longer you’re in that situation, the harder it becomes to cope with it.
Fortunately, it’s possible to cultivate resilience. To do so, it helps to exercise resiliency skills as often as possible, even for minor stressors. Marques recommends the following strategies.
Shift your thoughts
In stressful situations, try to balance out your thoughts by adopting a broader perspective. “This will help you stop using the emotional part of your brain and start using the thinking part of your brain. For example, if you’re asking for a raise and your brain says you won’t get it, think about the things you’ve done in your job that are worthy of a raise. You’ll slow down the emotional response and shift your mindset from anxious to action,” Marques says.
Approach what you want
“When you’re anxious, stressed, or burned out, you tend to avoid things that make you uncomfortable. That can make you feel stuck,” Marques says. “What you need to do is get out of your comfort zone and take a step toward the thing you want, in spite of fear.”
For example: If you’re afraid of giving a presentation, create a PowerPoint and practice it with colleagues. If you’re having conflict at home, don’t walk away from your partner — schedule time to talk about what’s making you upset.
Align actions with your values
“Stress happens when your actions are not aligned with your values — the things that matter most to you or bring you joy. For example, you might feel stressed if you care most about your family but can’t be there for dinner, or care most about your health but drink a lot,” Marques says.
She suggests that you identify your top three values and make sure your daily actions align with them. If being with family is one of the three, make your time with them a priority — perhaps find a way to join them for a daily meal. If you get joy from a clean house, make daily tidying a priority.
Tips for success
Practice the shift, approach, and align strategies throughout the week. “One trick I use is looking at my calendar on Sunday and checking if my actions for the week are aligned with my values. If they aren’t, I try to change things around,” Marques says.
It’s also important to live as healthy a lifestyle as possible, which will help keep your brain functioning at its best.
Healthy lifestyle habits include:
- getting seven to nine hours of sleep per night
- following a healthy diet, such as a Mediterranean-style diet
- aiming for at least 150 minutes of moderate-intensity activities (such as brisk walking) each week — and adding on strength training at least twice a week
- if you drink alcohol, limiting yourself to no more than one drink per day for women and two drinks per day for men
- not smoking
- staying socially connected, whether in person, by phone or video calls, social media, or even text messages.
Need resilience training?
Even the best athletes have coaches, and you might benefit from resilience training.
Consider taking an online course, such as this one developed by Luana Marques. Or maybe turn to a therapist online or in person for help. Look for someone who specializes in cognitive behavioral therapy, which guides you to redirect negative thoughts to positive or productive ones.
Just don’t put off building resilience. Practicing as you face day-to-day stresses will help you learn skills to help navigate when dark clouds roll in and seas get rough.
About the Author

Heidi Godman, Executive Editor, Harvard Health Letter
Heidi Godman is the executive editor of the Harvard Health Letter. Before coming to the Health Letter, she was an award-winning television news anchor and medical reporter for 25 years. Heidi was named a journalism fellow … See Full Bio View all posts by Heidi Godman
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD

A liquid biopsy for metastatic prostate cancer

Metastatic prostate cancer can progress in different ways. In some men the disease advances rapidly, while other men have slower-growing cancer and a better prognosis. Researchers are developing various tools for predicting how fast prostate cancer might progress. Among the most promising are assays that count circulating tumor cells (CTCs) in blood samples.
Prostate cancer spreads by shedding CTCs into the bloodstream, so higher counts in blood generally reflect worse disease. Sometimes referred to as a liquid biopsy, the CTC assay can help doctors decide if patients should get standard or more aggressive treatment. Just one CTC assay is currently on the market for prostate cancer. Called CellSearch, its use is so far limited to men with late-stage metastatic cancer for whom hormonal therapies are no longer effective.
Using CTC data
Hormonal therapies block testosterone, a hormone that drives prostate tumors to grow. Research shows that high CTC counts predict poorer survival and faster disease progression among patients with metastatic prostate cancer who become resistant to this form of treatment. But new research shows CTC counts are also predictive for early-stage metastatic prostate cancer that still responds to hormonal therapy.
Why is that important? Because the earlier doctors can predict a cancer’s trajectory, the better their ability to select patients who could benefit from more powerful (and potentially more aggressive) drug combinations or a clinical trial. Conversely, men who are older or frail might be treated less aggressively if doctors had better insights into their prognosis.
How the study was done
The investigators collected blood samples from 503 newly-diagnosed patients with hormonally-sensitive metastatic prostate cancer who had enrolled in a clinical trial with experimental hormonal therapies. The team collected baseline samples at trial registration, and then another set of samples after the treatments were no longer working. CTC counts were divided in three categories:
- more than 5 CTCs per 7.5 milliliters (mLs) of blood
- between 1 and 4 CTCs per 7.5 mLs of blood
- zero CTCs per 7.5 mLs of blood.
What the research showed
Results showed that men with higher baseline CTC counts fared worse regardless of which cancer drugs they were taking. Median survival for men with 5 or more CTCs per sample was 27.9 months compared to 56.2 months in men with 1 to 4 CTCs. There weren’t enough patient deaths among those with 0 CTCs to calculate a survival rate.
Similarly, higher CTC counts predicted faster onset of resistance to hormonal therapy: 11.3 months for men in the highest CTC category, compared to 20.7 months and 59 months for men with 1 to 4 and zero CTCs respectively. Importantly, higher CTC counts correlated with measures of prostate cancer severity, including PSA levels, numbers of metastases in bone, and other indicators.
Observations and comments
“This research emphasizes the continued emergence of CTCs in helping to determine outcomes and potentially treatment options for men with metastatic prostate cancer,” said Dr. Marc Garnick, the Gorman Brothers Professor of Medicine at Harvard Medical School and Beth Israel Deaconess Medical Center, and editor in chief of the Harvard Medical School Guide to Prostate Diseases.
“Still to be determined is how this type of testing compares with more traditional evaluations of disease advancement, such as x-rays, bone scans, and other types of imaging. Ready access to cancer cells in blood that, in turn, eliminate the need for more invasive biopsy procedures of metastatic deposits will be a welcome addition — especially if future studies show that CTCs inform more precise treatment choices.”
Dr. David Einstein, a medical oncologist specializing in genitourinary cancers at Beth Israel Deaconess Medical Center and assistant professor at Harvard Medical School, agreed with that assessment. “But the Holy Grail is finding predictive biomarkers [like CTCs] that tell you if patients will or will not benefit from particular treatments,” he added. “Answering these types of questions requires randomized clinical trials.”
About the Author

Charlie Schmidt, Editor, Harvard Medical School Annual Report on Prostate Diseases
Charlie Schmidt is an award-winning freelance science writer based in Portland, Maine. In addition to writing for Harvard Health Publishing, Charlie has written for Science magazine, the Journal of the National Cancer Institute, Environmental Health Perspectives, … See Full Bio View all posts by Charlie Schmidt
About the Reviewer
Marc B. Garnick, MD, Editor in Chief, Harvard Medical School Annual Report on Prostate Diseases; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Marc B. Garnick is an internationally renowned expert in medical oncology and urologic cancer. A clinical professor of medicine at Harvard Medical School, he also maintains an active clinical practice at Beth Israel Deaconess Medical … See Full Bio View all posts by Marc B. Garnick, MD

Gratitude enhances health, brings happiness — and may even lengthen lives

Several evenings a week, as Tyler VanderWeele gathers around the dinner table with his wife and two young kids, the family deliberately pauses during the meal to do something simple but profound. Each member shares several things for which they’re grateful — an act that VanderWeele, co-director of the Initiative on Health, Spirituality, and Religion at the Harvard T.H. Chan School of Public Health, feels changes his family dynamic for the better.
“I do think it makes a difference and can be a very powerful practice,” he says. “Even on those bad days where life seems difficult, that effort is worthwhile.”
Gratitude, health, and longevity
How can the power of gratitude affect our lives? Recent research has pointed to gratitude’s myriad positive health effects, including greater emotional and social well-being, better sleep quality, lower depression risks, and favorable markers of cardiovascular health. Now, new data from the long-term Nurses’ Health Study shows that it may extend lives.
“Gratitude has been one of the most widely studied activities contributing to well-being, but we couldn’t find a single prior study that looked at its effects on mortality and longevity, much to our surprise,” says VanderWeele, co-author of the new research.
What did the study look at?
Published July 2024 in JAMA Psychiatry, the new study drew on data from 49,275 women enrolled in the Nurses’ Health Study. Their average age was 79. In 2016, participants completed a six-item gratitude questionnaire in which they ranked their agreement with statements such as, “I have so much in life to be thankful for,” and “If I had to list everything I felt grateful for, it would be a very long list.”
Four years later, researchers combed through participants’ medical records to determine who had died. There were 4,608 deaths from all causes, as well as from specific causes such as cardiovascular disease, cancer, respiratory diseases, neurodegenerative disease, infection, and injury. Deaths from cardiovascular disease — a top killer of women and men in the United States — were the most common cause.
What did the researchers find?
Participants with gratitude scores in the highest third at the study’s start had a 9% lower risk of dying over the following four years than participants who scored in the bottom third. This did not change after controlling for physical health, economic circumstances, and other aspects of mental health and well-being. Gratitude seemed to help protect participants from every cause of death studied — including cardiovascular disease.
But what does this actually mean?
“A 9% reduction in mortality risk is meaningful, but not huge,” VanderWeele says. “But what’s remarkable about gratitude is that just about anyone can practice it. Anyone can recognize what’s around them and express thanks to others for what’s good in their life.”
While the study couldn’t pinpoint why gratitude is associated with longer life, VanderWeele believes several factors may contribute.
“We know that gratitude makes people feel happier. That in itself has a small effect on mortality risk,” he says. “Practicing gratitude may also make someone a bit more motivated to take care of their health. Maybe they’re more likely to show up for medical appointments or exercise. It may also help with relationships and social support, which we know contribute to health.”
What are the study’s limitations and strengths?
The study was observational. This means it can’t prove that gratitude helps people live longer — only that an association exists. And the particular sample of people analyzed is both the biggest strength and limitation of the research, VanderWeele says. All were older female nurses with high socioeconomic status. The vast majority were white.
“Does the longevity effect extend to men, to those who are younger, and to those with lower socioeconomic resources?” VanderWeele asks. “Those are all open questions.”
On the plus side, he says, the study sample’s large size is one of its biggest strengths. So is the extensive data gathered on potential confounding factors such as participants’ physical health, social characteristics, and other aspects of psychological well-being.
“Between the quality of the data and the size of the sample, we were able to provide reasonable evidence for this modest longevity effect,” he says.
Try this: Six questions to evoke gratitude
Not feeling especially grateful today? You have the power to change that. Asking yourself certain questions can evoke gratitude, such as
- What happened today that was good?
- What am I taking for granted that I can be thankful for?
- Which people in my life am I grateful for?
- What is the last book I read or movie, show, or social media clip I saw that I really appreciated, and why?
- What am I most looking forward to this week, month, and year, and why?
- What is the kindest thing someone has said or done lately?
Similarly, a few simple actions can infuse gratitude into your days. Try VanderWeele’s family routine of regularly expressing gratitude around the dinner table. Another well-known practice — that’s perhaps becoming forgotten in this digital age — is penning thank-you notes.
“I do think writing a thank-you note or gratitude letter gets your mind to dwell on something positive for a longer period, to think more deeply about it, because you have to put it not just in words, but in writing,” VanderWeele says. “It also deepens the relationship and builds that bond.”
One less-recognized but valuable gratitude practice is called a “savoring exercise,” which builds on aspects of mindfulness. All that’s required is “pausing, looking around you, and taking in and enjoying everything that’s good in your current setting,” VanderWeele says. “It’s not a big leap to go from recognizing the good to expressing gratitude for what you have.”
About the Author

Maureen Salamon, Executive Editor, Harvard Women's Health Watch
Maureen Salamon is executive editor of Harvard Women’s Health Watch. She began her career as a newspaper reporter and later covered health and medicine for a wide variety of websites, magazines, and hospitals. Her work has … See Full Bio View all posts by Maureen Salamon
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD

Alcohol and your health: Risks, benefits, and controversies

Cheers! Salud! Prost!
Drinking to one’s health is a common tradition. But it may also be self-defeating: the alcohol that’s part of many toasts can actually harm your health.
Of course, alcohol consumption extends well past toasts. For millions of people, it’s a regular part of the dining experience, social and sports events, celebrations, and milestones. Alcohol plays a key role in many religious traditions. And the alcoholic beverage industry is a major economic force, responsible for more than $250 billion in sales annually in the US.
But there are many downsides to drinking: some are likely familiar (spoiler alert: it’s not great for your liver) while others are less well appreciated. And concerns about the risks of even moderate drinking are on the rise.
The negative effects of alcohol
Here are some of the most common problems associated with alcohol consumption (especially if excessive):
- liver disease, including cirrhosis and life-threatening liver failure requiring a liver transplant
- a higher risk of high blood pressure, heart failure, and dementia
- an increased risk of cancer (more on this below)
- a higher risk of injury, especially from drunk driving and falls (homicides and suicides are also often alcohol-related)
- lapses in judgment — for example, people who are drunk may engage in risky sexual behavior or use other drugs
- an increased risk of depression, anxiety, and addiction: these problems may impact one’s ability to establish and maintain social relationships and employment
- fetal alcohol syndrome: alcohol can damage a baby’s developing brain and cause other developmental abnormalities
- alcohol poisoning: many people don’t realize that if you drink enough alcohol over a short period of time, it can be fatal.
Heavy drinking can also cause problems well beyond the health of the drinker — it can damage important relationships. It’s all too common that problem drinking disrupts bonds with a spouse, family members, friends, coworkers, or employers.
Alcohol and cancer: A growing concern
In recent decades, a number of studies have linked drinking to higher rates of cancer, including cancers involving the
- liver
- colon
- breast
- mouth
- throat and esophagus.
In many cases, even moderate drinking (defined below) appears to increase risk. Despite this, less than half of the US public is aware of any alcohol-cancer connection. That’s why the Surgeon General issued an advisory in January 2025 recommending that alcoholic beverages carry new labels warning of the alcohol-cancer link and highlighting that no safe low level of alcohol consumption has been established. Changing the labels as suggested by the Surgeon General will require congressional action that may never happen.
Current alcoholic beverage labels in the US warn of the risks of driving under the influence of alcohol, adverse effects on general health, and risks for a developing fetus — but there’s no mention of cancer.
Are there any health benefits to drinking alcohol?
Alcohol has long been considered a “social lubricant” because drinking may encourage social interaction. Having a drink while getting together with family or friends is often part of many special occasions.
And not so long ago there was general consensus that drinking in moderation also came with health advantages, including a reduced risk of cardiovascular disease and diabetes. More recently, this belief has been called into question.
Even among the positive studies, potential health benefits are often quite small. In addition, alcohol may reduce the risk of one condition (such as cardiovascular disease) while increasing the risk of another (such as cancer). So it’s hard to predict who might actually benefit and who may be harmed more than helped by alcohol consumption. And the balance of risk and benefit likely varies from person to person, based on individual factors such as genetics and lifestyle factors.
Is drinking some alcohol better than drinking none?
A number of studies suggest the answer may be yes. For example, a 2018 study found that light drinkers (those consuming one to three drinks per week) had lower rates of cancer or death than those drinking less than one drink per week or none at all.
More recent studies (all published in 2023) came to similar conclusions. For example:
- A study of nearly a million people followed for more than 12 years found that abstainers had higher rates of death and chronic disease (including cardiovascular disease, Alzheimer’s disease, and chronic lung disease) than light or moderate drinkers.
- Researchers reporting on more than half a million people found that nondrinkers had higher rates of death than moderate drinkers.
- An analysis combining findings from 22 prior studies concluded that people who drank wine had lower rates of cardiovascular disease and related death than those who did not.
By contrast, another 2023 study found similar rates of death between nondrinkers and light to moderate drinkers.
It’s worth noting that current guidelines advise against drinking alcohol as a way to improve health.
How much alcohol is too much?
The answer to this important question has varied over time, but current US guidelines recommend that men who drink should limit intake to two drinks/day or less and women who drink should have no more than one drink/day. The definitions for a drink in the US are the common serving sizes for beer (12 ounces), wine (5 ounces), or distilled spirits/hard liquor (1.5 ounces).
A number of experts have recommended revision of the guidelines toward lower amounts, as more studies have linked even moderate alcohol consumption to health risks. Predictably, the alcoholic beverage industry opposes more restrictive guidelines.
Of course, no one needs to wait for new guidelines or warning labels to curb their drinking. Many are exploring ways to cut back, including the Dry January Challenge or alcohol-free drinks.
What we don’t know: The significant limitations of alcohol-related health research
Nearly all large studies regarding alcohol’s impact on health assess associations, not causation. So a higher rate of certain cancers may be associated with more alcohol consumption, but that doesn’t prove alcohol caused the cancer.
In addition, most rely on self-reporting that may be inaccurate, do not analyze binge drinking, do not assess alcohol consumption over a lifetime, or do not account for the fact that some study subjects may change their alcohol consumption due to alcohol-related health problems. These limitations make it hard to know how much to rely on studies that find health risks (or benefits) to alcohol consumption.
The bottom line
Assessing the risks and benefits of alcohol consumption remains an active area of research that may lead to major changes in official guidelines or warning labels.
But here’s one thing that hasn’t changed: many people like to drink. Even with more restrictive guidelines or new warning labels, it’s likely that plenty of folks will accept the risks of drinking alcohol. Still, it’s important to know what those risks are.
So, stay tuned. You can expect to hear about more research, debate, and controversy in the near future regarding the potential risks and benefits of drinking, and how much — if any — is ideal.
About the Author
Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. … See Full Bio View all posts by Robert H. Shmerling, MD
An action plan to fight unhealthy inflammation
Although inflammation serves a vital role in the body’s defense and repair systems, chronic inflammation can cause more harm than good. And that may make you wonder: what can I do about it?
In fact, there’s a lot you can do. And you may already be doing it. That’s because some of the most important ways to fight inflammation are measures you should be taking routinely.
Let’s take a look at key elements of fighting chronic inflammation: prevention, detection, and treatment.
Six ways to prevent unhealthy inflammation
Six of the most effective ways to ward off inflammation are:
- Choose a healthy diet. Individual foods have a rather small impact on bodywide inflammation, so no, eating more kale isn’t likely to help much. But making sure you eat lots of fruits and vegetables, whole grains, healthy fats, and legumes — sometimes called an anti-inflammatory diet — may reduce inflammation and lower risk for chronic illnesses like diabetes and heart disease. Not only can these diets help reduce inflammation on their own, but replacing foods that increase inflammation (such as sugary drinks and highly processed foods) benefits your body, too.
- Exercise regularly.Physical activity may help counter some types of inflammation through regulation of the immune system. For example, exercise has anti-inflammatory effects on white blood cells and chemical messengers called cytokines.
- Maintain a healthy weight. Because excess fat in cells stimulates bodywide inflammation, avoiding excess weight is an important way to prevent fat-related inflammation. Keeping your weight in check also reduces the risk of type 2 diabetes, a condition that itself causes chronic inflammation.
- Manage stress. Repeatedly triggered stress hormones contribute to chronic inflammation. Yoga, deep breathing, mindfulness practices, and other forms of relaxation can help calm your nervous system.
- Do not smoke. Toxins inhaled in cigarette smoke trigger inflammation in the airways, damage lung tissue, and increase the risk of lung cancer and other health problems.
- Try to prevent inflammatory conditions, such as
- Infection: Take measures to avoid infections that may cause chronic inflammation. HIV, hepatitis C, and COVID-19 are examples. Practicing safer sex, not sharing needles, and getting routine vaccinations are examples of effective preventive measures.
- Cancer: Get cancer screening on the schedule recommended by your doctors. For example, colonoscopy can detect and remove polyps that could later become cancerous.
- Allergies: By avoiding triggers of asthma, eczema, or allergic reactions you can reduce the burden of inflammation in your body.
Do you need tests to detect inflammation?
While testing for inflammation is not routinely recommended, it can be helpful in some situations. For example, tests for inflammation can help to diagnose certain conditions (such as temporal arteritis) or monitor how well treatment is controlling an inflammatory condition (such as Crohn’s disease or rheumatoid arthritis).
However, there are no perfect tests for inflammation. And the best way to know if inflammation is present is to have routine medical care. Seeing a primary care physician, reviewing your medical history and any symptoms you have, having a physical examination, and having some basic medical tests are reasonable starting points. Such routine care does not typically include tests for inflammation.
How is inflammation treated?
At first glance, treating unhealthy, chronic inflammation may seem simple: you take anti-inflammatory medications, right? Actually, there’s much more to it than that.
Anti-inflammatory medicines can be helpful to treat an inflammatory condition. And we have numerous FDA-approved options that are widely available — many in inexpensive generic versions. What’s more, these medicines have been around for decades.
- Corticosteroids, such as prednisone, are the gold standard. These powerful anti-inflammatory medicines can be lifesaving in a variety of conditions, ranging from asthma to allergic reactions.
- Other anti-inflammatory medicines can also be quite effective for inflammatory conditions. Ibuprofen, naproxen, and aspirin — which may already be in your medicine cabinet — are among the 20 or so nonsteroidal anti-inflammatory drugs (NSAIDs) that come as pills, tablets, liquids taken by mouth, products applied to skin, injections, and even suppositories.
Yet relying on anti-inflammatory medicines alone for chronic inflammation is often not the best choice. That’s because these medicines may need to be taken for long periods of time and often cause unacceptable side effects. It’s far better to seek and treat the cause of inflammation. Taking this approach may cure or contain many types of chronic inflammation. It may also eliminate the need for other anti-inflammatory treatments.
For example, chronic liver inflammation due to hepatitis C infection can lead to liver scarring, cirrhosis, and eventually liver failure. Medicines to reduce inflammation do not solve the problem, aren’t particularly effective, and may cause intolerable side effects. However, treatments available now can cure most cases of chronic hepatitis C. Once completed, there is no need for anti-inflammatory treatment.
Similarly, among people with rheumatoid arthritis, anti-inflammatory medicines such as ibuprofen or steroids may be a short-term approach that helps ease symptoms, yet joint damage may progress unabated. Controlling the underlying condition with medicines like methotrexate or etanercept can protect the joints and eliminate the need for other anti-inflammatory drugs.
The bottom line
Even though we know that chronic inflammation is closely linked to a number of chronic diseases, quashing inflammation isn’t the only approach, or the best one, in all cases.
Fortunately, you can take measures to fight or even prevent unhealthy inflammation. Living an “anti-inflammatory life” isn’t always easy. But if you can do it, there’s an added bonus: measures considered to be anti-inflammatory are generally good for your health, with benefits that reach well beyond reducing inflammation.
About the Author
Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. … See Full Bio View all posts by Robert H. Shmerling, MD

Should you be tested for inflammation?

Let’s face it: inflammation has a bad reputation. Much of it is well-deserved. After all, long-term inflammation contributes to chronic illnesses and deaths. If you just relied on headlines for health information, you might think that stamping out inflammation would eliminate cardiovascular disease, cancer, dementia, and perhaps aging itself.
Unfortunately, that’s not true.
Still, our understanding of how chronic inflammation can impair health has expanded dramatically in recent years. And with this understanding come three common questions: Could I have inflammation without knowing it? How can I find out if I do? Are there tests for inflammation? Indeed, there are.
Testing for inflammation
A number of well-established tests to detect inflammation are commonly used in medical care. But it’s important to note these tests can't distinguish between acute inflammation, which might develop with a cold, pneumonia, or an injury, and the more damaging chronic inflammation that may accompany diabetes, obesity, or an autoimmune disease, among other conditions. Understanding the difference between acute and chronic inflammation is important.
These are four of the most common tests for inflammation:
- Erythrocyte sedimentation rate (sed rate or ESR). This test measures how fast red blood cells settle to the bottom of a vertical tube of blood. When inflammation is present the red blood cells fall faster, as higher amounts of proteins in the blood make those cells clump together. While ranges vary by lab, a normal result is typically 20 mm/hr or less, while a value over 100 mm/hr is quite high.
- C-reactive protein (CRP). This protein made in the liver tends to rise when inflammation is present. A normal value is less than 3 mg/L. A value over 3 mg/L is often used to identify an increased risk of cardiovascular disease, but bodywide inflammation can make CRP rise to 100 mg/L or more.
- Ferritin. This is a blood protein that reflects the amount of iron stored in the body. It’s most often ordered to evaluate whether an anemic person is iron-deficient, in which case ferritin levels are low. Or, if there is too much iron in the body, ferritin levels may be high. But ferritin levels also rise when inflammation is present. Normal results vary by lab and tend to be a bit higher in men, but a typical normal range is 20 to 200 mcg/L.
- Fibrinogen. While this protein is most commonly measured to evaluate the status of the blood clotting system, its levels tend to rise when inflammation is present. A normal fibrinogen level is 200 to 400 mg/dL.
Are tests for inflammation useful?
In certain situations, tests to measure inflammation can be quite helpful.
- Diagnosing an inflammatory condition. One example of this is a rare condition called giant cell arteritis, in which the ESR is nearly always elevated. If symptoms such as new, severe headache and jaw pain suggest that a person may have this disease, an elevated ESR can increase the suspicion that the disease is present, while a normal ESR argues against this diagnosis.
- Monitoring an inflammatory condition. When someone has rheumatoid arthritis, for example, ESR or CRP (or both tests) help determine how active the disease is and how well treatment is working.
None of these tests is perfect. Sometimes false negative results occur when inflammation actually is present. False positive results may occur when abnormal test results suggest inflammation even when none is present.
Should you be routinely tested for inflammation?
Currently, tests of inflammation are not a part of routine medical care for all adults, and expert guidelines do not recommend them.
CRP testing to assess cardiac risk is encouraged to help decide whether preventive treatment is appropriate for some people (such as those with a risk of a heart attack that is intermediate — that is, neither high nor low). However, for most people evidence suggests that routine CRP testing adds relatively little to assessment using standard risk factors, such as a history of hypertension, diabetes, smoking, high cholesterol, and positive family history of heart disease.
So far, only one group I know of recommends routine testing for inflammation for all without a specific reason: companies selling inflammation tests directly to consumers.
Inflammation may be silent — so why not test?
It’s true that chronic inflammation may not cause specific symptoms. But looking for evidence of inflammation through a blood test without any sense of why it might be there is much less helpful than having routine health care that screens for common causes of silent inflammation, including
- excess weight
- diabetes
- cardiovascular disease (including heart attacks and stroke)
- hepatitis C and other chronic infections
- autoimmune disease.
Standard medical evaluation for most of these conditions does not require testing for inflammation. And your medical team can recommend the right treatments if you do have one of these conditions.
The bottom line
Testing for inflammation has its place in medical evaluation, and in monitoring certain health conditions such as rheumatoid arthritis. But it’s not clearly helpful as a routine test for everyone. A better approach is to adopt healthy habits and get routine medical care that can identify and treat the conditions that contribute to harmful inflammation.
About the Author
Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. … See Full Bio View all posts by Robert H. Shmerling, MD

New surgery for benign prostate hyperplasia provides long-lasting benefits

Most men over 50 will develop an enlarged prostate. Also called benign prostatic hyperplasia (BPH), this bothersome condition makes it hard to urinate and can eventually lead to other problems, such as infections, kidney stones, and bladder damage, if left untreated. Many different BPH therapies are available, including medications and various types of surgery.
One of the newer surgical options, called aquablation, trims excess prostate tissues with highly pressurized jets of saline. Doctors perform aquablation in the operating room while looking at the prostate gland on an ultrasound machine. Patients are put under general anesthesia, so they don’t feel any pain during the procedure.
Men typically have to urinate through a catheter for about 24 hours after surgery until swelling of the urethra (the tube through which urine flows out of the bladder) subsides. Aquablation is gaining in popularity — in part because, unlike other more traditional BPH treatments, it can preserve normal ejaculation.
In September, researchers published a study showing that improvements in urinary function from aquablation were still holding up after five years.
Results of data analysis
The study assessed long-term data from two clinical trials. The first, called the WATER trial (for Waterjet Ablation Therapy for Endoscopic Resection of Prostate Tissue) launched in 2015 and enrolled 116 men with prostates ranging up to 80 cubic centimeters. The second trial, WATER II, launched in 2017 and enrolled 101 men with prostates ranging between 80 and 150 cubic centimeters. (Normal prostates range from 25 to 30 cubic centimeters in size.) Enrolled patients had a median age of 66 in the WATER study and 68 in WATER II. In addition, 92% of men in the WATER trial were sexually active, as were 75% of the men in WATER II.
Both clinical trials used the so-called International Prostate Symptom Score (IPSS) to measure treatment-related improvements in urinary functioning and quality of life. Calculated based on how patients rate their symptoms on a standardized questionnaire, IPSS scores fall into three categories: mild symptom scores range from 1 to 7; intermediate symptom scores range from 8 to 18; and scores greater than 19 indicate severe symptoms.
When they first enrolled in the trials, men in the WATER and WATER II studies reported average IPSS scores of 22.9 and 23.3 respectively. Five years later, the average respective scores were much lower: 7.0 and 6.8. The average length of hospital stay was 1.4 days in the WATER group and 1.6 days for the WATER II group. Only 1% of men were taking BPH medications after five years, and fewer than 5% had been surgically re-treated.
Another randomized control trial, WATER III, is currently underway in Europe. That trial compares aquablation with a more established type of BPH surgery, prostate enucleation, which uses a laser to remove obstructing tissues. Six-month data reported in 2023 showed that men in either group had comparable symptom improvements.
However, 98% of men in the prostate enucleation group had ejaculatory dysfunction. That side effect is caused by damage to delicate tissues around the bladder neck that propel semen out of the body. Semen therefore flows back into the bladder, a condition called retrograde ejaculation. None of the men in the aquablation group reported ejaculatory problems.
A word of caution
Aquablation can result in extended bleeding, cautions Dr. Heidi Rayala, an assistant professor of urology at Harvard Medical School and a member of the Harvard Medical School Guide to Prostate Diseases advisory board. That’s because unlike other types of surgery for BPH, including prostate enucleation, aquablation doesn’t cauterize tissues with heat. “I tell my patients to expect some blood in the urine for about four to six weeks after the procedure,” Dr. Rayala said.
Moreover, aquablation may be unsuitable for some men who take blood thinners to prevent blood from clotting, according to Dr. Rayala. Appropriate candidates for the surgery must be able to “safely discontinue anticoagulant medications during post-operative healing, given the bleeding risk,” Dr. Rayala said. Still, aquablation is an excellent option for most men, Dr. Rayala said, especially those with medium to large prostates “who want a durable solution with a lower risk of sexual side effects.”
“These early results are encouraging, but limited by a relatively small number of patients,” said Dr. Marc Garnick, the Gorman Brothers Professor of Medicine at Harvard Medical School and Beth Israel Deaconess Medical Center, and editor in chief of the Harvard Medical School Guide to Prostate Diseases. “Further evidence with a significantly larger number of patients and longer follow-up will help to support this new method of reducing prostate tissue as an important treatment option.”
About the Author

Charlie Schmidt, Editor, Harvard Medical School Annual Report on Prostate Diseases
Charlie Schmidt is an award-winning freelance science writer based in Portland, Maine. In addition to writing for Harvard Health Publishing, Charlie has written for Science magazine, the Journal of the National Cancer Institute, Environmental Health Perspectives, … See Full Bio View all posts by Charlie Schmidt
About the Reviewer
Marc B. Garnick, MD, Editor in Chief, Harvard Medical School Annual Report on Prostate Diseases; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Marc B. Garnick is an internationally renowned expert in medical oncology and urologic cancer. A clinical professor of medicine at Harvard Medical School, he also maintains an active clinical practice at Beth Israel Deaconess Medical … See Full Bio View all posts by Marc B. Garnick, MD

Shining light on night blindness

Animals renowned for their outstanding night vision include owls, cats, tarsiers (a tiny primate in Southeast Asia) — and even the dung beetle.
But humans? Not so much.
Over time, many people suffer from night blindness, also known as nyctalopia. This condition makes seeing in dim or dark settings difficult because your eyes cannot adjust to changes in brightness or detect light.
What are the dangers for those experiencing night blindness?
Night blindness is especially problematic and dangerous when driving. Your eyes cannot adjust between darkness and the headlights of oncoming vehicles, other cars may appear out of focus, and your depth perception becomes impaired, which makes it difficult to judge distances.
Night blindness also may affect your sight at home by making it hard for your vision to quickly adjust to a dark room after turning off the lights. “This can cause people to bump into furniture or trip and suffer an injury,” says Dr. Isabel Deakins, an optometrist with Harvard-affiliated Massachusetts Eye and Ear.
What happens in the eye to create night blindness?
The ability to see in low-light conditions involves two structures in the eye: the retina and the iris.
The retina, located in the back of the eye, contains two types of light-detecting cells called cones and rods. The cones handle color vision and fine details while the rods manage vision in dim light.
The iris is the colored part of your eye. It contains muscles that widen or narrow the opening of your pupil to adjust how much light can enter your eyes.
If your irises don’t properly react, the pupils can dilate and let in too much light, which causes light sensitivity and makes it hard to see in bright light. Or your pupils may remain too small and not allow in enough light, making it tough to see in low light.
What causes night blindness?
Night blindness is not a disease but a symptom of other conditions. “It’s like having a bruise on your body. Something else causes it,” says Dr. Deakins.
Several conditions can cause night blindness. For instance, medications, such as antidepressants, antihistamines, and antipsychotics, can affect pupil size and how much light enters the eye.
Eye conditions that can cause night blindness include:
- glaucoma, a disease that damages the eye’s optic nerves and blood vessels
- cataracts, cloudy areas in the lens that distort or block the passage of light through the lens
- dry eye syndrome.
However, one issue that raises the risk of night blindness that you can’t control is age. “Our eyes react more slowly to light changes as we age, and vision naturally declines over time,” says Dr. Deakins. “The number of rods in our eyes diminish, pupils get smaller, and the muscles of the irises weaken.”
What helps if you have night blindness?
If you notice any signs of night blindness, avoid driving and get checked by an eye care specialist like an optometrist or ophthalmologist. An eye exam can determine if your eyeglass prescription needs to be updated.
“Often, a prescription change is enough to reduce glare when driving at night," says Dr. Deakins. “You may even need separate glasses with a stronger eye prescription that you wear only when driving at night.”
Adding an anti-reflective coating to your lens may help to cut down on the glare of the headlights of an oncoming car. However, skip the over-the-counter polarized driving glasses sold at many drug stores. "These may help cut down on glare, but they don't address the causes of night blindness," says Dr. Deakins.
An eye exam also will identify glaucoma or cataracts, which can be treated. Glaucoma treatments include eyedrops, laser treatment, or surgery. Cataracts are corrected with surgery to replace the clouded lens with an artificial one. Your eye care specialist can also help identify dry eye and recommend treatment.
Ask your primary care clinician or a pharmacist if any medications that you take may cause night blindness. If so, it may be possible to adjust the dose or switch to another drug.
Three more ways to make night driving safer
You also can take steps to make night driving safer. For example:
- Wash the lenses of your glasses regularly. And take them to an optician to buff out minor scratches.
- Keep both sides of your front and rear car windshields clean so that you can see as clearly as possible.
- Dim your dashboard lights, which cause glare, and use the night setting on your rearview mirror.
About the Author

Matthew Solan, Executive Editor, Harvard Men's Health Watch
Matthew Solan is the executive editor of Harvard Men’s Health Watch. He previously served as executive editor for UCLA Health’s Healthy Years and as a contributor to Duke Medicine’s Health News and Weill Cornell Medical College’s … See Full Bio View all posts by Matthew Solan
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD

No-cost, low-cost, and bigger splurges for climate-conscious gifts

Looking for gifts to give or donate this year? Climate-conscious gifts come in many guises. They may directly support our environment, for example, or aim to reduce fossil fuel use and electronic, textile, and food waste. Or they might offer enjoyable, creative ways to connect, reuse, and recycle — and possibly even regift.
“Our purchases and choices impact our climate and planet,” notes Dr. Wynne Armand, a physician and associate director of the Massachusetts General Hospital Center for the Environment and Health. Small steps like these do help, she says, even when the complex issues of climate change leading to health-compromising pollution, extreme weather, and a stressed planet feel so large and overwhelming.
“Unquestionably, we need bold, strong leaders to seek policy changes that address these problems at a systems level. But, as individuals we can make a difference through small steps,” says Dr. Armand. “Our choices help drive cultural and market shifts that hopefully push our neighbors, businesses, and policy leaders in the right direction.”
Four climate-conscious principles for gifting
- Channel the 5 Rs. Refuse, reduce, reuse, repurpose, and only then recycle. Say no to excess. Comic sections from print newspapers or beautiful images from last year’s calendars or magazines make great envelopes and gift wrap. If you’re choosing clothes, consider buying upcycled clothing or at resale shops, as appropriate.
- Beware of greenwashing. Eco-consciousness is big business, and the benefits of what you buy may be questionable. If you have a small lawn that needs infrequent maintenance, says Dr. Armand, keeping a trusty (albeit gas-fueled) mower could be a better choice for the planet than buying an electric mower, when factoring in upstream costs of natural resources and the carbon footprint required to manufacture and ship the new — and toss out the not-so-old. (Alternatively, maybe it’s time to replant that lawn with wildflowers and vegetables?)
- Skip what’s not needed. A new backpack crafted from water bottles? Another sweater to add to a closetful? If there’s no apparent need, think twice about purchases.
- Double down on experiences and connection. Think concert tickets, museum passes, or energetic options like rock-climbing gym passes and outdoor skills classes. “Gifts of experience are great, especially for people who already have all they need. If you buy for two or try a skills swap you also get to enjoy that time together,” says Dr. Armand.
25 climate-conscious gifts
Below are 25 suggestions for climate-conscious giving intended to work with many budgets.
Small but mighty climate-conscious gifts
1. Soft, warm sweaters, thick socks, or puffer vests can help people turn down the heat, saving energy resources and money.
2. Rechargeable batteries reduce materials and packaging waste.
3. An electric kettle, induction hot plate, or toaster oven can help limit indoor pollutants from gas stoves.
4. Perfectly Good Food: A Totally Achievable Zero Waste Approach to Home Cooking aims to pare back food waste and is available online.
5. Shop local artisans and craft fairs rather than buying online.
6. Plants brighten any room and help scrub the air: choose easy-care varieties, such as succulents, colorful coleus, and some herbs.
7. Protect the natural world: birds, bees, and other insects could use your help. Consider a small bird feeder that attaches to a window, a bee house, gardening tools, or seeds for a pollinator garden of colorful flowers.
8. Donate to national or worldwide climate or environmental organizations, local green spaces, and local conservation groups.
9. Gift green bonds for companies that support renewable energy — do your research, though, because greenwashing can be an issue.
10. Secret gifter-giftee swaps with large groups save sanity and throttle back waste.
Bigger splurges on climate-conscious gifts
11. When appliances reach the end of useful life, consider replacing gas stoves, water heaters, washers, dryers, and similar items with electric versions.
12. Plan a week of nearby tours and events with friends or family instead of flights and faraway travel.
13. Gift clothes and tools to enjoy the natural world: for example, warm, waterproof clothing and hiking boots, cross-country skis or skates, good binoculars for bird-watching.
14. Composters (or a weekly composting service subscription) recycle food scraps and organic waste into soil-enriching “black gold.”
15. Electric bikes may be a boon if they reduce reliance on vehicles using fossil fuels.
16. Help fund energy-efficient heat pumps or renewable solar energy.
17. Substantial donations and sustaining donor gifts to climate-conscious organizations can help in many ways.
No-cost climate-conscious gifts
18. Offer to gather information on big-ticket items in the big splurges section, including state and federal rebates and 0% loans for heat pumps, energy-efficient furnaces, solar panels, and energy-efficient appliances.
19. Teach a skill one-on-one, such as home repair, skating, chess, training for a mud run, knitting, cooking, orienteering, or gardening, or organize skills swaps with friends.
20. Gift the human power needed to replant portions of a lawn with vegetables or pollinator plants, or make a rain garden (note: automatic download) to help divert storm water.
21. Combine a no-cost reminder of the environmental benefits of no-mow May and leave the leaves campaigns with an offer to help peel back these layers come spring.
22. Friends often want to gift one another — costly generosity that can prompt last-minute candle-buying. As an alternative, gather a small group of friends for a clothing, accessories, and candle swap of new, never-took-the-price-tag-off, nearly new, and well-loved items.
23. Offer a DIY nature or bird walk for two. Try the free Pl@ntnet and Merlin apps if you can’t tell a pin oak from a petunia or a robin from a California condor.
24. If you buy for a ton of people, buy in bulk and figure out how to parcel it out in more sustainable packaging.
25. Make dinner, fudge, or another treat with friends — not completely free, but always a great way to gather your community.
About the Author

Francesca Coltrera, Editor, Harvard Health Blog
Francesca Coltrera is editor of the Harvard Health Blog, and associate editor of multimedia content for Harvard Health Publishing. She is an award-winning medical writer and co-author of Living Through Breast Cancer and The Breast Cancer … See Full Bio View all posts by Francesca Coltrera
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD